What is Covid-19?
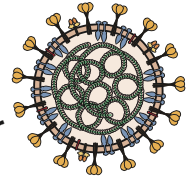
CORONA VIRUS DISEASE (COVID 19) is caused by a member of the coronavirus family that has never been encountered before. Like other coronaviruses, it has transferred to humans from animals. The World Health Organisation (WHO) has declared it a pandemic.
Coronaviruses are important human and animal pathogens. At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. It rapidly spread, resulting in an epidemic throughout China, followed by an increasing number of cases in other countries throughout the world. In February 2020, the World Health Organization designated the disease COVID-19, which stands for coronavirus disease 2019. The virus that causes COVID-19 is designated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); previously, it was referred to as 2019-nCoV.
The new coronavirus, provisionally called 2019-nCoV, that originated in China has spread globally with approximately seven lakh confirmed cases worldwide and death toll of more than 30,800 till the time of writing this article. Slowly COVID 19 is spreading in India and now case burden is more than thousand and death toll is 25 till now and increasing day by day.
What was the origin of the virus?
The virus was first isolated by infection of cells in culture with broncho-alveolar wash from a patient in Wuhan with pneumonia. The infected cells showed cytopathic effects, and staining of cells with an antibody to coronavirus NP protein, which is conserved among coronaviruses, revealed intracellular staining.
The complete genome sequence of this isolate was determined (29,891 bases) and comparison with genomes of other coronaviruses revealed that it is most closely related (96.2% identity) with viral RNA from a Rhinolophus affinis bat obtained in Yunnan Province in 2013. This finding means that both viruses have a common ancestor in bats. Recall that SARS-CoV also originated in bats. Many coronaviruses circulate in bats and more are likely to cross into humans in the future.
How the virus entered humans from bats is unknown.
Mode of Transmission
According to current evidence, COVID-19 virus is transmitted between people through respiratory droplets and contact routes.1
Droplet transmission occurs when a person is in in close contact (within 1 m) with someone who has respiratory symptoms (e.g. coughing or sneezing,) and is therefore at risk of having his/her mucosae (mouth and nose) or conjunctiva (eyes) exposed to potentially infective respiratory droplets (which are generally considered to be > 5-10 μm in diameter). Droplet transmission may also occur through fomites in the immediate environment around the infected person. Therefore, transmission of the virus can occur by direct contact with infected people and indirect contact with surfaces in the immediate environment or with objects used on the infected person (e.g. stethoscope or thermometer).
Airborne transmission is different from droplet transmission as it refers to the presence of microbes within droplet nuclei, which are generally considered to be particles < 5μm in diameter, and which result from the evaporation of larger droplets or exist within dust particles. They may remain in the air for long periods of time and be transmitted to others over distances greater than 1 meter.
In the context of COVID-19, airborne transmission may be possible in specific circumstances and settings in which procedures that generate aerosols are performed (i.e. endotracheal intubation, bronchoscopy, open suctioning, administration of nebulized treatment, manual ventilation before intubation, turning the patient to the prone position, disconnecting the patient from the ventilator, non-invasive positive-pressure ventilation, tracheostomy, and cardiopulmonary resuscitation). In analysis of 75,465 COVID-19 cases in China, airborne transmission was not reported.
There is some evidence that COVID-19 infection may lead to intestinal infection and be present in faeces. However, to date only one study has cultured the COVID-19 virus from a single stool specimen. There have been no reports of faecal−oral transmission of the COVID-19 virus to date.
Implications of recent findings of detection of COVID-19 virus from air sampling . These initial findings need to be interpreted carefully.
A recent publication in the New England Journal of Medicine has evaluated virus persistence of the COVID-19 virus.9 In this experimental study, aerosols were generated using a three-jet Collison nebulizer and fed into a Goldberg drum
under controlled laboratory conditions. This is a high-powered machine that does not reflect normal human cough conditions. Further, the finding of COVID-19 virus in aerosol particles up to 3 hours does not reflect a clinical setting in which aerosol-generating
procedures are performed—that is, this was an experimentally induced aerosol-generating procedure.
There are reports from settings where symptomatic COVID-19 patients have been admitted and in which nov COVID 19 RNA was detected in air samples. In addition, it is important to note that the detection of RNA in environmental samples based on PCR-based assays is not indicative of viable virus that could be transmissible.
Based on the available evidence, including the recent publications mentioned above, WHO continues to recommend droplet and contact precautions for those people caring for COVID-19 patients and contact and airborne precautions for circumstances and settings in which aerosol generating procedures are performed. These recommendations are consistent with other national and international guidelines, including those developed by the European Society of Intensive Care Medicine and Society of Critical Care Medicine1 and those currently used in Australia, Canada, and United Kingdom.
At the same time, other countries and organizations, including the US Centers for Diseases Control and Prevention and the European Centre for Disease Prevention and Control, recommend airborne precautions for any situation involving the care of COVID-19 patients, and consider the use of medical masks as an acceptable option in case of shortages of respirators (N95, FFP2 or FFP3).1
Current WHO recommendations emphasize the importance of rational and appropriate use of all PPE, not only masks, which requires correct and rigorous behavior from health care workers, particularly in doffing procedures and hand hygiene practices. WHO also recommends staff training on these recommendations, as well as the adequate procurement and availability of the necessary PPE and other supplies and facilities. Finally, WHO continues to emphasize the utmost importance of frequent hand hygiene, respiratory etiquette, and environmental cleaning and disinfection, as well as the importance of maintaining physical distances and avoidance of close, unprotected contact with people with fever or respiratory symptoms.
Period of infectivity
The interval during which an individual with COVID-19 is infectious is uncertain. Most data informing this issue are from studies evaluating viral RNA detection from respiratory and other specimens. However, detection of viral RNA does not necessarily indicate the presence of infectious virus.
Viral RNA levels appear to be higher soon after symptom onset compared with later in the illness; this raises the possibility that transmission might be more likely in the earlier stage of infection, but additional data are needed to confirm this hypothesis.
The duration of viral shedding is also variable; there appears to be a wide range, which may depend on severity of illness. In one study of 21 patients with mild illness (no hypoxia), 90 percent had repeated negative viral RNA tests on nasopharyngeal swabs by 10 days after the onset of symptoms; tests were positive for longer in patients with more severe illness. In another study of 137 patients who survived COVID-19, the median duration of viral RNA shedding from oropharyngeal specimens was 20 days (range of 8 to 37 days) .
The reported rates of transmission from an individual with symptomatic infection vary by location and infection control interventions. According to a joint WHO-China report, the rate of secondary COVID-19 ranged from 1 to 5 percent among tens of thousands of close contacts of confirmed patients in China. Among crew members on a cruise ship, 2 percent developed confirmed infection . In the United States, the symptomatic secondary attack rate was 0.45 percent among 445 close contacts of 10 confirmed patients.
Transmission of SARS-CoV-2 from asymptomatic individuals (or individuals within the incubation period) has also been described. However, the extent to which this occurs remains unknown. Large-scale serologic screening may be able to provide a better sense of the scope of asymptomatic infections and inform epidemiologic analysis; several serologic tests for SARS-CoV-2 are under development.
What are the symptoms this COVID 19?
People may be sick with the virus for 1 to 14 days before developing symptoms. According to the WHO, the most common symptoms of Covid-19 are fever, tiredness and a dry cough. Some patients may also have a runny nose, sore throat, nasal congestion and aches and pains or diarrhoea. Some people report losing their sense of taste and/or smell. About 80% of people who get Covid-19 experience a mild case – about as serious as a regular cold – and recover without needing any special treatment. More rarely, the disease can be serious and even fatal.
About one in six people, the WHO says, become seriously ill. The elderly and people with underlying medical problems like high blood pressure, heart problems or diabetes, or chronic respiratory conditions, cancer patients, patients getting immuno-suppressants are at a greater risk of serious illness from Covid-19.
Specific symptoms:
- A high temperature – you feel hot to touch on your chest or back
- A new continuous dry cough and sore throat- this means you’ve started coughing repeatedly
- Shortness of breath in severe cases
- A loss of smell and taste may be the early symptom of COVID-19 infection, according to a latest report by a leading American professional association of medical specialists.
Is there any treatment?
As this is viral pneumonia, antibiotics are of no use. The antiviral drugs we have against flu will not work, and there is currently no vaccine. Recovery depends on the strength of the immune system.
Should I go to the doctor if I have a temperature or a cough?
Yes. You should go for testing your samples in the nearby center for diagnosis. At the same time anyone with symptoms should stay at home as self quarantine for at least 7 days. If you live with other people, they should stay at home for at least 14 days, to avoid spreading the infection outside the home. This applies to everyone, regardless of whether they have travelled abroad.
HOW TO PREVENT THIS DREADED COVID 19?
There’s currently no vaccine to prevent coronavirus disease (COVID-19). Only way to stop this epidemic is to stop man to man transmission. That’s why Govt of India and other states have announced complete lock down.
You can protect yourself and help prevent spreading the virus to others if you:
Do
Wash your hands regularly for 20 seconds, with soap and water or alcohol-based hand rub
Cover your nose and mouth with a disposable tissue or flexed elbow when you cough or sneeze
Avoid close contact (1 meter or 3 feet) with other people
Stay home and self-isolate from others
Don’t
Touch your eyes, nose, or mouth if your hands are not clean
